What we already knew about the antibodies against SARS-COV-2
In our first study on patients who had recovered from COVID-19, we saw that some patients had more antibodies in their blood, and that in others the level of antibodies declined very quickly.
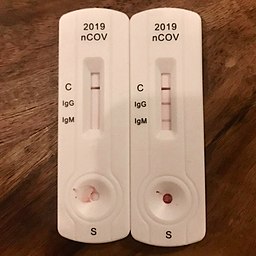
Moreover, looking at different groups of patients all over the world (including ours), it appears that about 10% of patients infected by SARS-COV-2 have detectable levels of antibodies against the N protein of the virus.
Our experiments
We decided to study the difference between those patients who recovered from COVID-19 and had detectable antibodies, and those who had not.
In particular, we analysed the blood of our patients looking at
- the levels of neutralising antibodies, able to “capture” the virus and avoid the infection of more cells
- the activity of immune cells called T cells in response to different proteins of the virus: Surface (S), Nucleocapsid (N), Membrane (M), and ORF-7a-2
- the levels of molecules called cytokines and chemokines that, produced during infection, transmit messages between the infected cells and the immune system
Our results
- We found that the majority of patients (about 70%) who did not have antibodies against the N protein, had neutralising antibodies that recognised the S protein. It is known that the production of antibodies against different viral proteins happens at different times during infection, and, like in waves, the levels of a new type of antibody start to increase when the previous ones start to fade. In our study, however, the patients with high levels of antibodies against N antibodies had also high levels of neutralising antibodies against S, while those with low levels of anti-N had also low levels of neutralising antibodies.
- We also found that T cells from different groups of patients have their own “favourite protein”: T cells from patients with antibodies against N react stronger against the S protein, while T cells from patients without antibodies against N, react against the Membrane protein (M), but not against S.
- When we measured the levels of 20 cytokines and chemokines, we found that only one of them was different between the two groups: beta-NGF (β-NGF). Rita Levi Montalcini discovered this protein and its functions as a nerve growth factor in the 50s, and she was awarded the Nobel Prize for Physiology and Medicine in 1986.
What does β-NGF have to do with COVID-19?
This protein has been studied since the 50s, and it has been discovered that it serves several functions in the immune response, and that it is produced by B and T cells. Interestingly, its production increases during inflammation, and cells can respond to it using two different receptors:
- TrkA induces cell activity and proliferation
- p75 can cause cell death
When the levels of β-NGF in the blood are high, some cells produce more TrkA to be able to respond more efficiently to it. The interaction between β-NGF and TrkA has already been studied in the context of other respiratory diseases caused by viruses, like the respiratory syncytial virus (RSV) and human rhinovirus (HRV).
We found that those patients who did not produce antibodies against the N protein had lower levels of β-NGF, and their T cells had lower amounts of TrkA, and were, therefore, less active. This difference was particularly relevant in one subtype of T cells that help B cells produce antibodies. It seems, therefore that the message transmitted by β-NGF and received by TrkA is very important also for the immune response against SARS-CoV-2.
Why are these results important?
This is only one of the possible differences between people producing different amounts of antibodies against SARS-CoV-2, and the fact that the immune response against this virus does not have the same intensity or the same duration in all of us is surely the result of many factors. We need more studies with more patients of different ethnicities to complete this huge puzzle.
Understanding why the immune response is so variable in all its components – not only antibodies – is extremely important to organise the vaccination programs and decide which groups are more at risk and should be considered the top priority. Vaccines are still our most valuable tool to prevent severe COVID-19 and to limit the spread of the virus, and they should be used in the wisest possible way.
Bibliography
The β-NGF/TrkA signalling pathway is associated with the production of anti-nucleoprotein IgG in convalescent COVID-19, Usai C et al., Frontiers in Immunology 2022 https://doi.org/10.3389/fimmu.2021.813300
Great work. The TrkA part doesn’t surprise me since, as you write, it has been studied for other viral infections as well.
LikeLike
Thank you!
LikeLike